
The Michigan Association for Local Public Health is advocating for a transformative vision of public health, one that accounts for the complexities of today’s diverse communities and the ever-evolving landscape of health needs.
The Yours, Mine, and Ours — Public Health series highlights how our state's public health agencies keep us healthy, safe, and informed about issues impacting physical and mental health in our communities, homes, workplaces, and schools. The series is made possible with funding from the Michigan Association for Local Public Health.
In the wake of the COVID-19 pandemic, public health departments across Michigan are confronting new challenges that have fundamentally altered how public health is practiced. The pandemic highlighted significant vulnerabilities within the system, from gaps in communication to inadequate preparedness for future health crises. Today, as the world adjusts to a new normal, the Michigan Association for Local Public Health (MALPH) is playing a crucial role in reimagining what public health should look like in a post-pandemic world.
MALPH advocates for a transformative vision of public health, one that accounts for the complexities of today’s diverse communities and the ever-evolving landscape of health needs. With a focus on addressing the social determinants of health and creating more resilient public health infrastructures, MALPH’s new vision emphasizes collaboration, adaptability, and the need to improve health literacy across Michigan.

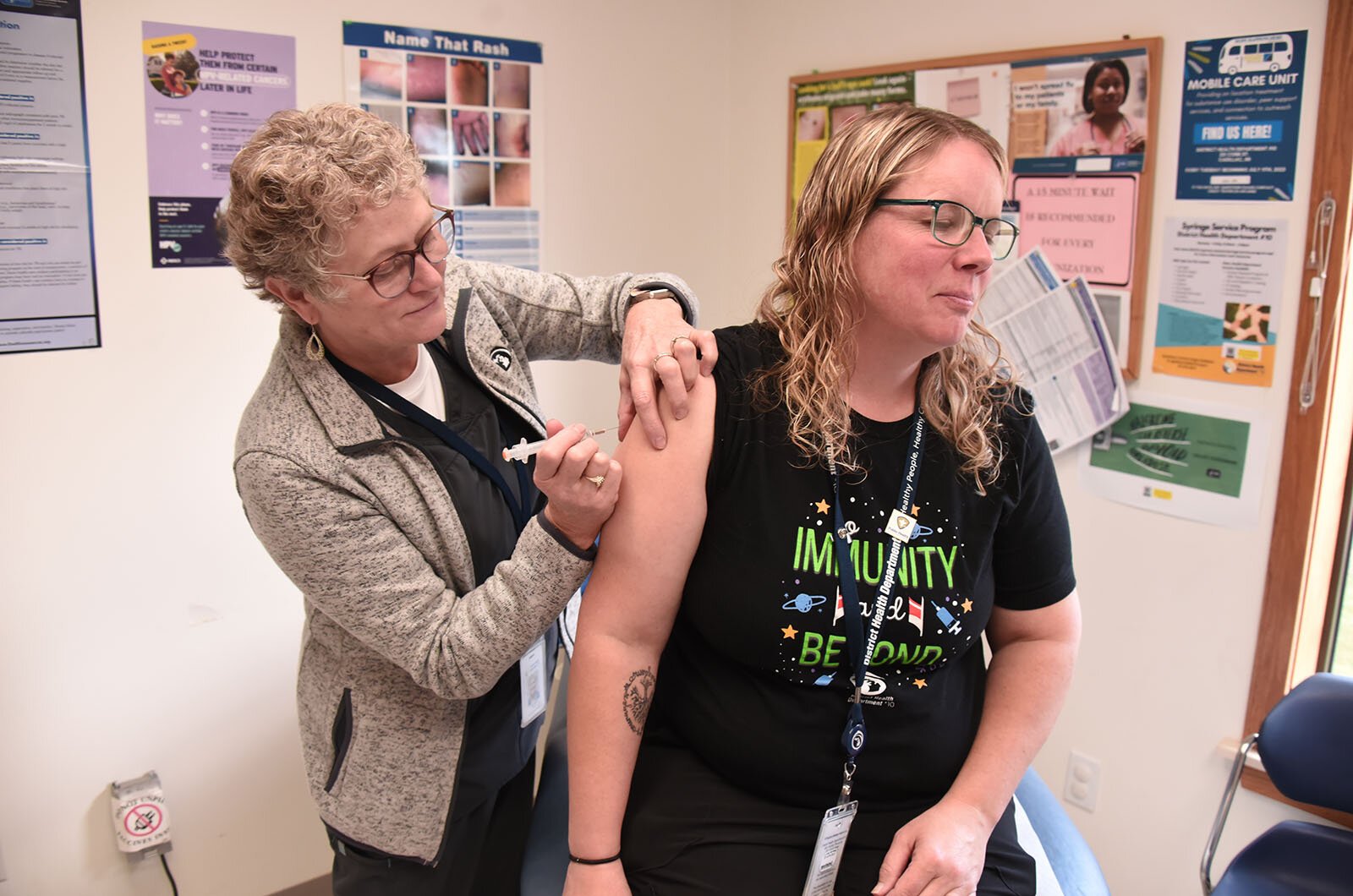
“Some people’s only interaction with us is because of the pandemic, so many people think that’s all public health is, but it’s so much more than that,” says Kevin Hughes, president of MALPH’s executive committee and health officer with District Health Department #10. “MALPH is advocating for the improvement of public health outreach, public health literacy in communities, and improving the overall understanding of all that public health does have to offer communities.”
These efforts are part of a broader push to educate both the public and policymakers on the full scope of public health, which extends far beyond pandemics and emergency preparedness.
A wake-up call for public health
The pandemic was a wake-up call for public health officials, revealing that the system was not adequately prepared for the scale of the crisis. From overburdened hospitals to inconsistent messaging around preventive measures, the weaknesses became glaringly apparent. Now, as Michigan looks toward the future, public health leaders are working to fortify their operations — not only to be ready for the next major public health emergency but also to rethink how everyday public health functions can be made more efficient and responsive to community needs.
One of the key priorities is improving public health literacy — both at the individual and community levels. Health literacy refers to the public’s ability to obtain,

understand, and use health information to make informed decisions. It’s a critical factor in shaping positive health outcomes for individuals and communities alike.
“It’s about more than just getting information out. We have to think about how we in the health sector are communicating risk and data,” says Dr. Laura Power, director of the Office of Public Health Practice at the University of Michigan. “We have to continue working both within the health sector and outside of it to improve communication but also provide communities with the tools to understand, verify information, and ask questions.”
The pandemic demonstrated that simply providing information isn’t enough. Effective communication requires ensuring that the information is accessible, accurate, and understandable to people with varying levels of health literacy. This is especially important in communities with limited access to healthcare resources, where misinformation can quickly spread.

Redefining public health
MALPH’s vision for the future of public health in Michigan is centered on addressing the root causes of health disparities. One major component of this new vision is an increased focus on the social determinants of health — factors like housing, education, and economic stability, which have a profound impact on health outcomes. Hughes emphasizes that public health must go beyond disease prevention and treatment to encompass a broader range of social factors that influence health.
“Public health is not just about immunizations; there’s so much more education and prevention work that we have to do in communities,” says Hughes.
By addressing the underlying social determinants of health, public health leaders hope to improve not just life expectancy but also the quality of life for Michigan

residents. Hughes believes that an integrated approach will help address chronic health conditions like heart disease, diabetes, and hypertension, which disproportionately affect vulnerable populations.
Norm Hess, executive director of MALPH, echoes this sentiment.
“Improving life expectancy is not just about adding years to life; it’s about adding life to those years,” says Hess. “We need to focus on helping our seniors thrive in their later years while also encouraging younger generations to take steps now that will ensure their health as they age.”
Post-pandemic challenges and opportunities
The COVID-19 pandemic not only exposed gaps in the public health system but also exacerbated existing health issues, such as the rise in obesity, substance abuse, and mental health crises. These challenges are no longer isolated problems affecting individuals — they are now community-wide issues that require a coordinated, systemic response.
“We have to recognize that health isn’t just the absence of disease,” says Power. “Positive mental health, economic health, and social connections contribute to the ability for people to thrive. These are all critical components of health.”
Local health departments are now facing these challenges on a daily basis, often with limited resources. Staffing shortages in particular have become a significant concern, with many departments struggling to recruit and retain qualified personnel.
“We’re seeing staffing issues, workforce issues, and many resources are slowly starting to dry up and go away,” says Hughes. “Everybody seems to also be having a harder time recruiting and retaining people.”
Funding is another critical issue facing public health departments. Much of the funding is tied to specific programs, which may not align with local priorities or the unique needs of each community. Hess stresses the need for more flexible funding streams that would allow local health departments to allocate resources where they are most needed.
“Our future success depends on building a more robust public health infrastructure with flexible funding that allows us to respond to the unique needs of each community,” says Hess.
Building a collaborative future for public health
To address these challenges, MALPH is calling for greater collaboration between public health departments and non-traditional partners, such as local governments, housing authorities, schools, and community-based organizations.
“The pandemic provided a moment to have a long-overdue conversation about local public health’s role in helping everyone live longer, healthier lives,” says Hess. “It’s a high-stakes conversation because unhealthy communities struggle to grow and attract new residents.”
MALPH envisions a future in which public health departments are integrated more deeply into the fabric of their communities, working hand-in-hand with other sectors to create environments that promote health and well-being. By addressing the social determinants of health and building stronger, more adaptable public health infrastructures, Michigan’s public health system will be better equipped to meet the challenges of the future.
“The world has changed, and a strengthened sense of community and connection to public health is necessary,” says Power. “But with the right funding and a commitment to equity, Michigan’s public health leaders can create a new vision for public health in the state.”
Brianna Nargiso, a graduate of Howard University and Mercer University, specializes in media, journalism, and public health. Her work has appeared in The Root, 101 Magazine, and Howard University News Service, covering profiles, politics, and breaking news. A Hearst journalism award nominee and active member of the National Association for Black Journalists, she has also worked with Teach for America and the Peace Corps. Now a doctoral candidate at American University, Brianna is dedicated to advancing social justice, public health and education on a global scale.
Photos by John Russell.
The Yours, Mine, and Ours — Public Health series highlights how our state’s public health agencies keep us healthy, safe, and informed about issues impacting physical and mental health in our communities, homes, workplaces, and schools. The series is made possible with funding from the Michigan Association for Local Public Health.






